
In America, racial and ethnic health disparities impact millions of people and lead to unequal health outcomes in minority populations. Studies have indicated that minority populations suffer more from chronic diseases, inferior quality health care, and poor health compared to Whites. These health disparities are deep-rooted and accompanied by economic inequality, cultural disparities, historical discrimination, and widespread healthcare issues.
For home care agencies, those statistics translate to real problems: patients who have difficulty ceasing the care they need, caregivers who struggle with structural barriers, and providers mired in trying to address system issues. Closing those disparities in health outcomes isn’t a matter of doing the right thing or complying with regulations; it’s a matter of providing high-quality care that is individualized to each patient’s unique needs, regardless of background.
But how do you do it? That’s where person-centered care comes in. Through a focus on individualized care, education in diverse cultures, and effective communication, home care professionals can make a real difference in the care of minority patients. This blog discusses how person-centered care can help close health outcome disparities between minorities and mainstream America and what agencies can do to narrow the gap. Let’s take the first step!
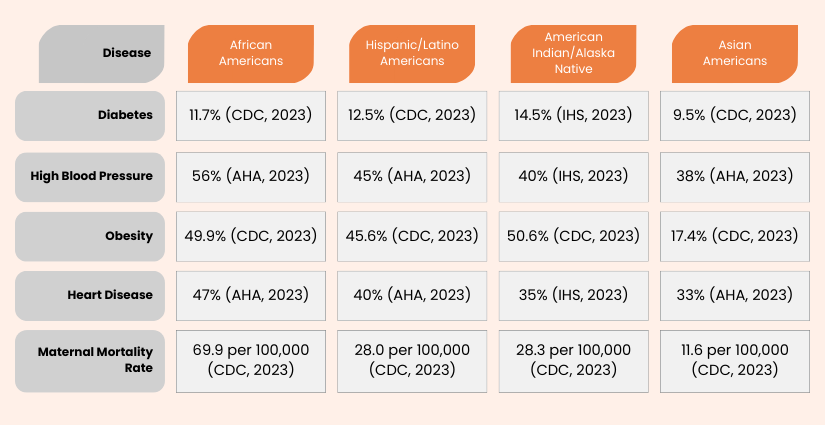
Research has repeatedly shown that racial and ethnic minorities in the US suffer more health issues, have a higher incidence of preventable illness, and have lower life expectancy. Some statistics make an overwhelming case for better healthcare for minorities:
A person-centered care model is a care model that prioritizes the person’s values, preferences, and individualized needs over the one-size-fits-all approach. Instead of treating symptoms, caregivers consider the entire person—culture, lifestyle, and personal health outcomes.
For minority patients, this is particularly critical because it ensures that minority care is individualized to address the unique health threats, cultural traditions, and care barriers minority populations experience.
Through person-centered care, caregivers can be able to:
– Erin Heath, Caregiver, Home Instead
The most significant barrier to effective care for minority patients is the lack of culturally sensitive communication. Too many patients are misunderstood or unheard of by clinicians who do not take the time to understand their cultural knowledge of health and illness.
Caregivers can bridge this gap by:
For instance, a black patient with hypertension will more readily follow herbal medication rather than pharmaceuticals because they mistrust the latter. A caregiver cannot deny their choice but instead helps them develop culturally acceptable nutrition and lifestyle changes that are part of care planning.
Health disparities are generally a result of the lack of patient control of medical decision-making. Minority patients often report being coerced into treatment plans they do not understand or agree with.
A person-centered care approach promotes collaborative decision-making to engage patients in their care. This includes:
By involving patients in decisions about their care, home care services can improve treatment for minority patients and maintain trust and long-term investment in the overall healthcare experience.
For English-speaking patients, lack of proper communication is a significant barrier to quality care. Inability to understand may lead to medication mismatches, failed appointments, and failure to adhere to a treatment plan.
To enhance healthcare outcomes for minorities, caregivers should:
For example, a Hispanic patient with limited English proficiency may not assign value to the significance of diabetes control. A person-centered care approach would include providing Spanish-language materials and ensuring caregivers communicate effectively to facilitate their care planning.
Social factors, including income, housing stability, and accessibility to transportation, dictate many determinants of health outcomes for minorities. A person-centered care approach recognizes these barriers and works toward reversing them.
Caregivers can help a patient by doing the following:-
For example, if an elderly Black patient struggles to attend medical appointments due to transportation issues, their caregiver can work with community services to make the necessary transportation arrangements. This helps patients have stable care and improves the outcomes of minority patients.
Representative caregivers can help improve care for minorities. Patients feel at ease when caregivers are knowledgeable about their culture and background. Home care agencies can help by:
When patients see caregivers who resemble them and share their experiences, they will be more involved in their care and trust the healthcare system.
New telehealth technologies, artificial intelligence (AI), and digital health technology are revolutionizing how we deliver care. For racial and ethnic minorities, these technologies are eradicating most of the barriers to receiving care, making it easier to extend care and ensure quality. With technology, providers can craft care plans that address the unique needs of minority groups and enhance care for minority patients.
Artificial intelligence transforms minority healthcare by enhancing early disease detection, personalizing treatment plans, and eliminating diagnosis bias. Here’s how AI is making a difference:
Telehealth provides a powerful mechanism for improving the care of minorities, especially for rural and inner-city populations who lack services. In this way:
Wearable Technology – Wearable devices and mHealth apps have empowered the underrepresented patient through digital technologies as they take more control over health. Such innovations allow a care model to be person-centric by encouraging and educating people on effective self-management, thus enabling and educating them.
Smartwatches use wearable health tracking to monitor patients’ vital signs, detect early warning signs of chronic disease, and alert the practitioner if intervention is needed.
Improving care for minority patients requires more than recognizing disparities; it requires intentional action. Embracing person-centered care principles can help close the racial and ethnic disparities gap, improve minority healthcare outcomes, and build an inclusive, equitable healthcare system.
A person-centered approach is suitable for patients and improving relationships between caregivers and patients, caregiver job satisfaction, and overall effectiveness in healthcare. Every small step—listening more carefully, learning about a client’s culture, or demanding better resources—adds to significant change.
Putting care planning, cultural understanding, and patient empowerment at the forefront, home care agencies can be the leaders in improving minority care outcomes and quality care for all, regardless of origin.
Related Blogs:
Addressing Client Demographics with Targeted Training Programs
Shaping the Future of Caregiving: Key Trends and Innovations
Contact us to inquire about our state-wise training courses and take the first step towards upskilling your team with a 14-day free trial!